Continuity of Care: the optimal experience for healthcare
Digital health has driven significant transformative advancement in the healthcare sector. The ultimate goal is to improve health outcomes, tackle disparities in access to care, and promote inclusivity for all populations. One way to work is by adopting the concept of continuity of care, which encompasses the coordination and integration of healthcare services across multiple providers and settings.
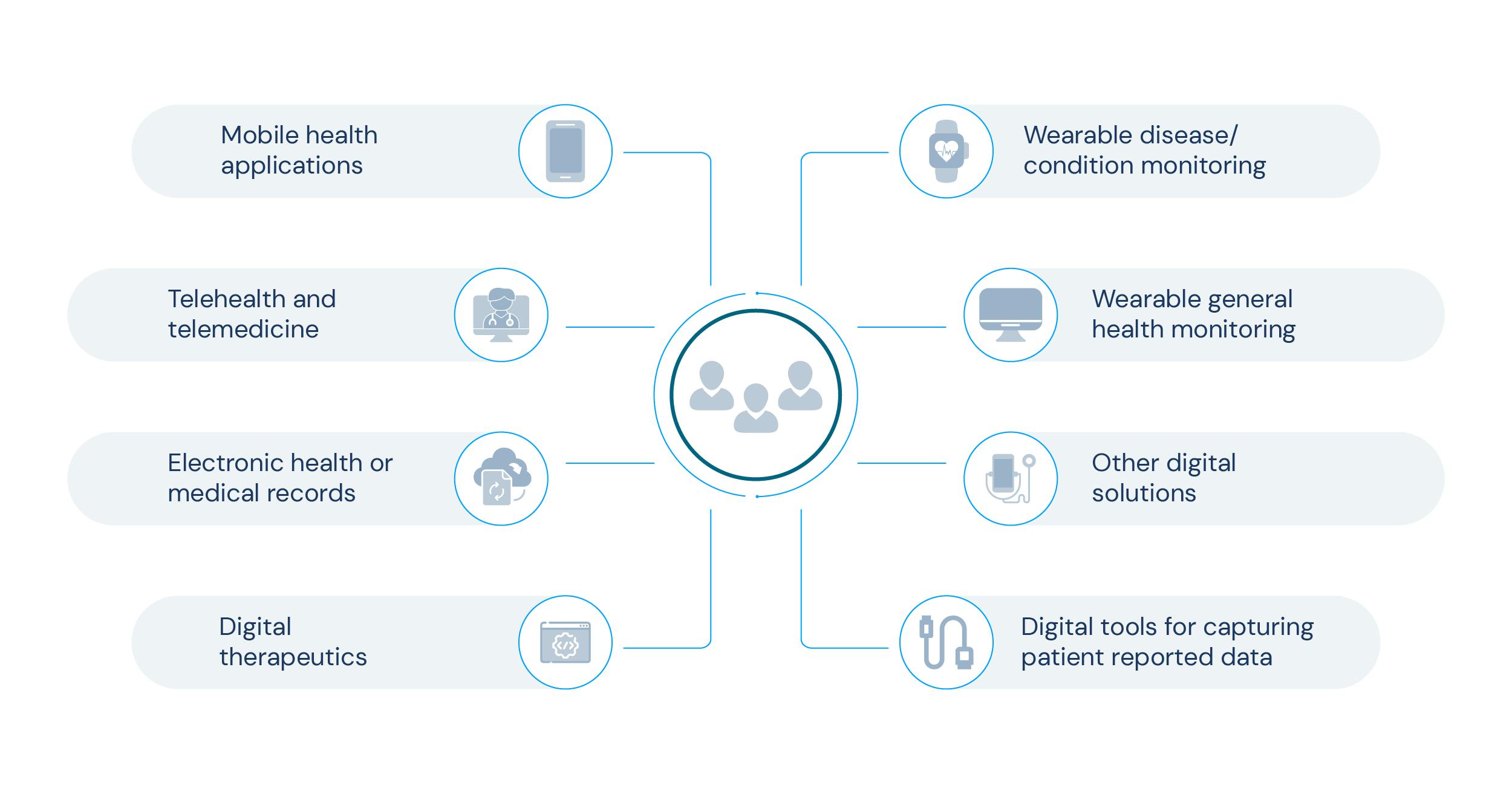
The world of digitally transformed health is leading the way with artificial intelligence, machine learning, digitally-mediated diagnostics and treatment, telemedicine, and consumer-centred mobile health applications. These more recent developments promise to enhance patient outcomes, promote early diagnoses and interventions, and engage patients in practising a healthier lifestyle. However, the full potential of digital health remains elusive and providers have to fully understand how it can really change healthcare for the better.
Even the most sophisticated technologies and innovative solutions will have little impact on clinical and practical outcomes if the healthcare system isn't prepared for this type of intervention. This is where the concept of continuity of care can act as a model for optimal healthcare services.
Continuity of Care and its mission
Adopting digital health models has proven its growing importance to every stakeholder across the healthcare industry. Telehealth and telemedicine services, for example, take down the barriers of access to healthcare, allowing providers to deliver care to more people while also improving health outcomes. Research analysis has shown that the use of telehealth has increased 38 times since before the COVID-19 pandemic. This ongoing growth creates numerous opportunities for the technology innovation sector to fill the existing gaps.
The continuous digital transformation within healthcare makes having a digital overview of every process and patient experience a natural process. Therefore providing ‘Continuum of Care’, or Continuity of Care, is definitely one of the strategies the Digital Health field should bet on.
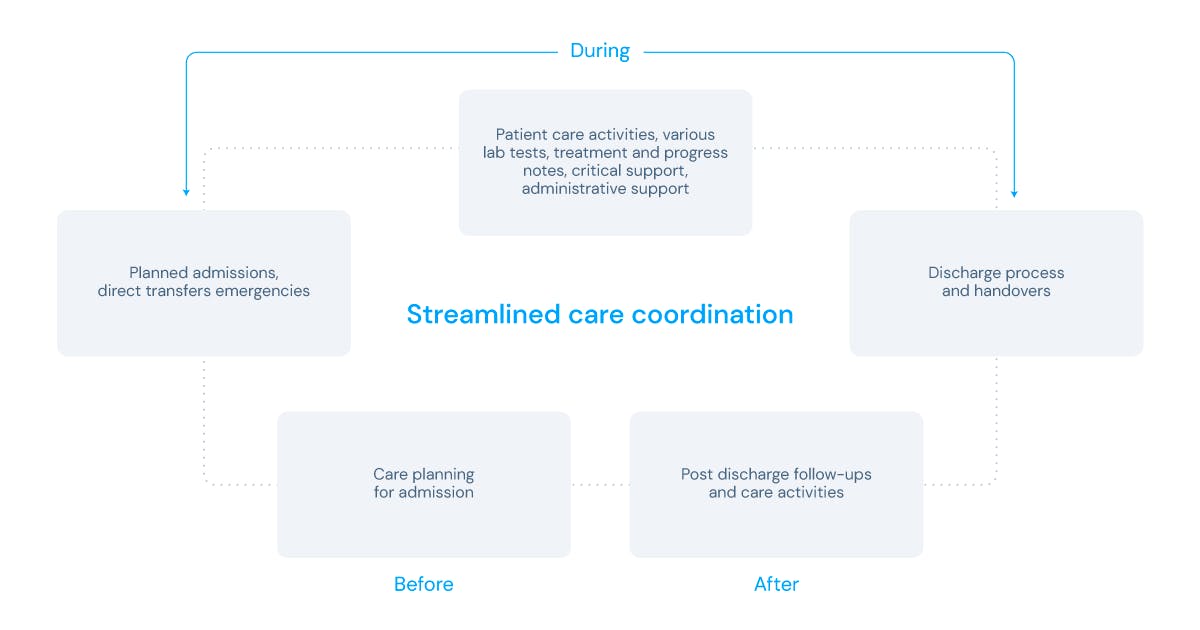
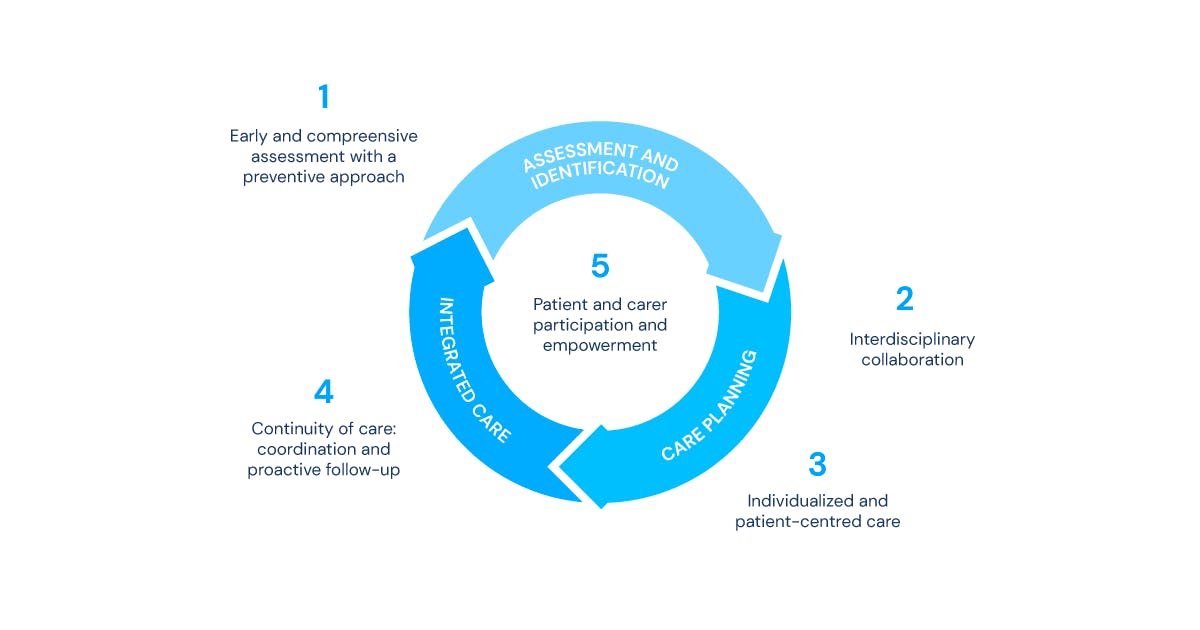
According to the Royal College of General Practitioners (RCGP), continuity of care is defined by the degree to which a person experiences an ongoing relationship with healthcare providers and receives coordinated clinical care while progressing across different parts of the healthcare system. It’s called continuity (or continuum) of care as it implies three phases: relational, management, and informational.
- Relational continuity involves seeing the same healthcare professionals or team over time and building trust and familiarity.
- Management continuity ensures that a patient's care is coordinated and managed effectively across different providers and services.
- Informational continuity refers to the seamless flow of information and records between healthcare providers, ensuring patients receive the most accurate and effective care possible.
By prioritising continuity of care, healthcare providers can help improve patient outcomes and ensure that patients receive the highest quality care possible. Moreover, the concept of continuity of care also envisions the best way to provide healthcare as efficiently as possible, while reducing overall costs within the business by making sure that the process is being followed seamlessly and on loop.At a global level, this involves the dedication of time for all health-related matters, and consistency to deliver a patient’s needs and preferences. Following a continuum of care throughout the patient journey means better care provided and more commitment of patients that are seeing their long-term needs met. To implement this series of integrated services are required to enable continuity of care and balance all the health information needed.
The benefits of Continuity of Care
The implementation of continuity of care strategies has proven to be a successful way to improve the quality of care on many health fronts. In the US, for example, there have been many projects and digital health strategies that have proven to enhance the quality and reduce the variation of acute stroke care.
This resulted in a turning point in the delivery of hospital-based stroke and heart-disease care, leading to significant improvements in national certification and standardisation of stroke treatments, as well as to prevention processes and outcomes across the country. Having the structure and guidelines for the detection and transportation of suspected stroke patients by emergency medical services, as well as ensuring proper discharge to the most appropriate post-acute care setting based on medical need, provides the highest quality of care a patient expects and needs; as well as it keeps medical operations efficient and balanced.
As patients transition from inpatient to outpatient care, the focus often shifts from acute to chronic conditions, requiring increased attention and management of chronic illnesses. From a digital health standpoint, having a continuity of care mindset will provide a better care experience, which ultimately enables better health outcomes. This model of digital continuity of care offers numerous benefits for both patients and providers and some of them are listed below.
Improved care coordination
Digital health tools can help healthcare providers coordinate care across different providers and care settings. By sharing patient data and information in real time, providers can more effectively manage chronic conditions, prevent medical errors, and ensure that patients receive the most appropriate care at the right time.
Enhanced patient engagement
Enabling patients to take a more active role in their care is also a huge step provided by the use of digital tools in healthcare. For example, patient portals and mobile health apps allow patients to access their medical records, communicate with providers, schedule appointments, and track their symptoms and health outcomes. This increased engagement can also lead to better adherence to treatment plans, improved health outcomes, and greater patient satisfaction.
Increased efficiency
Digital health tools are also beneficial for streamlining administrative tasks, such as scheduling appointments, processing insurance claims, and managing patient data. This can save time and resources, allowing providers to focus more on patient care.
Better outcomes
As a result of improving care coordination, patient engagement, and efficiency, continuity of care in a digital health setting will also lead to better health outcomes. A great example are patients with chronic conditions, who may experience fewer hospital readmissions, reduced healthcare costs, and improved quality of life.
The role of Preventive Care
The concept of continuity of care and preventive care can almost be seen as homologous, although they are not. As mentioned previously, this model of care ensures a higher quality of healthcare while maintaining an efficient operational line. However, a big part of the process of healthcare delivery also consists of prevention.
While continuity of care emphasises the ongoing relationship between patients and providers and all the coordinated care processes that occur during the care journey; preventive care encompasses all measures taken to prevent illnesses. In a certain matter, continuity of care can also play a crucial role in facilitating preventive care.
When patients have an ongoing relationship with a healthcare provider they trust, they are more likely to get regular health check-ups, exams and other preventive actions. Healthcare providers who are familiar with a patient's medical history and risk factors are also better equipped to provide personalised recommendations for preventive care. Which also leads to the benefits of having a patient-centred model in the first place.
For example, for patients who live with the complexity of multimorbidity, a streamlined, coordinated care will create a health setting that seeks to treat them holistically, like shown in the image below.
Digital Solutions to the rescue
Prevention has proven to be the best solution for treating patients at risk of chronic illnesses. Therefore, many healthcare organisations are implementing a transition from a sick care (interventive) model to a preventive one, where resources are laid out in favour of preventive measures. For many stakeholders in the industry, there’s a collective hope that a preventive care model will be the solution to lifting the burden of chronic diseases. Consequently, providers will be able to give higher-value care while enabling the best outcomes.
If the last couple of years has taught us something, it’s the potential of digital solutions. The digital transformation in healthcare has been showcasing its world of possibilities and rapidly paving the way towards preventive care, which is also boosting the concept of continuity of care. One way to do this is by building and scaling digital therapeutics to help improve the management of chronic illnesses.
With the recent digital health technology releases, the fundings for digital therapeutics have grown up to 134% since 2021. The potential seems to be evident, both in clinical and medical terms as well as economical ones, gathering for all parties involved.
More commonly known as DTx, digital therapeutics are evidence-based solutions driven by software that aid in prevention, management or treatment for medical disorders and disease. In a sense, DTx are patient-centred solutions which help patients self-manage with the support the implementation of mHealth solutions, such as apps, sensors, and IoT, AI or VR technologies. These interventions can aid the continuum of care in multiple ways, for example:
1. Providing patients with remote access to care
By enabling access from anywhere with an internet connection, DTx solutions allow patients to receive care outside of traditional healthcare settings; which can be especially beneficial for patients with chronic conditions who require ongoing management and monitoring.
2. Enhancing patient engagement
DTx solutions can be designed to engage and motivate patients to take an active role in their care. A good example are the interactive apps that can provide patients with personalised feedback, mobile reminders, and other tools to help them achieve their health goals. Also, using other strategies such as gamification to incentivise and challenge patients, can promote adherence in healthier life choices but also help them keep track of their health.
3. Improving outcomes
DTx interventions have shown to improve outcomes for a range of medical conditions, especially chronic ones, including diabetes, hypertension, and mental health conditions. By providing patients with access to evidence-based interventions, DTx can help patients manage their conditions more effectively and achieve better health outcomes.
4. Facilitating data sharing
Like most digital solutions, DTx can facilitate data sharing between patients and healthcare providers, which aids providers to make more informed decisions about patient care. For example, patients can use DTx solutions to track their symptoms and share this data in real-time with their providers, allowing them to monitor their condition more closely. Also, by using advanced analytics and health data it's possible to, collectively, predict and prevent global health events.
Augmented Telemedicine for Continuity of Care
As healthcare costs continue to rise and healthcare networks are becoming more consolidated, there is a growing need to leverage digital health solutions to create more affordable, high-quality, and accessible healthcare options. This means developing seamless and scalable solutions that are dedicated to protecting patients’ continuity of care. Augmented Telemedicine, for example, is a concept that has great potential to leverage those solutions.
A digital solution that aligns physicians, hospitals and stakeholders is one that creates an easy, insightful and improved patient journey. At knokcare, we believe in creating the right patient journey, designed specifically for each chronic disease or targeted population, enabling continuity of care as a form of prevention. With our platform Panacea, we can change how healthcare providers use their systems to aid their patients and, consequently, improve their health holistically.
Our applied concept of Augmented Telemedicine uses big data to strengthen medical insights and create health status clusters to show relevant clinical points, which can lead to personalised programs not only in hospitals and practices, but also for enterprises. The idea of adopting data integration in healthcare goes beyond connecting patients, providers and insurers in a circular matter. This convergence of high technology with healthcare creates efficiencies across the continuum of care and enhances the power of innovation.
Providing patients with more access to their health journey, easing processes and workloads for providers, and breaking inefficiencies for stakeholders is the ultimate goal in the digital and smart health world. When setting up and developing healthcare solutions, we’re also reshaping a new relationship between patients, healthcare providers and health systems in general.
Sources:
Telehealth: A quarter-trillion-dollar post-COVID-19 reality?
How Digital Health should focus on Continuum of Care experience for patients?
Continuity of Care work at RCGP
Three ways digital transformation is accelerating the shift to preventive care
The health benefits and business potential of digital therapeutics