Remote Patient Monitoring: taking a healthier approach to ageing
Introduction
Remote patient monitoring (RPM) is a healthcare technology that has the potential to revolutionise elderly care. By combining wearables, sensors, and mobile devices, RPM allows healthcare providers to monitor patients remotely outside traditional healthcare settings. As the global population ages, elderly care has become increasingly important since this population often presents complex health needs and requires more frequent medical attention than younger populations.
To take proper care of the elderly, healthcare providers constantly need to adjust their services to new diseases, technologies and medications. In this article, we will explore how RPM has the potential to improve elderly care in various ways. Through early detection of health problems, improved patient outcomes and reduced healthcare costs, this modern model of care can revolutionise how the elderly receive health services.
The Benefits of Remote Patient Monitoring for Elderly Care
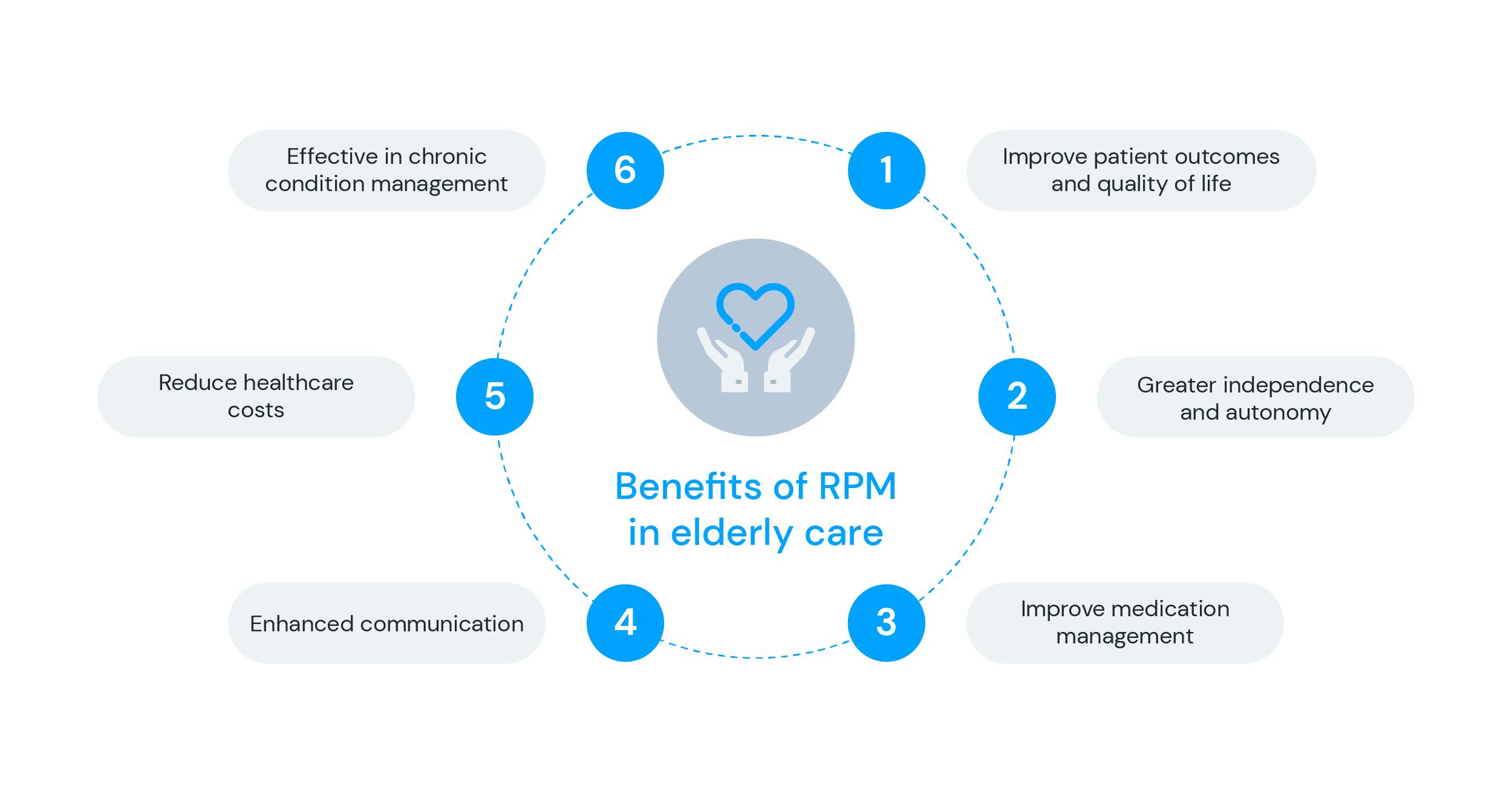
With several different applications to elderly care, RPM offers benefits that can revolutionise the way society takes care of the older population. By continuously monitoring patients outside of traditional healthcare settings such as hospitals and clinics, providers can detect early warning signs of health issues and diseases to intervene before they escalate into more serious medical problems. Early detection can lead to better treatment outcomes, reduced overall healthcare costs and improved quality of life for elderly patients.
Additionally, remote patient monitoring can provide elderly patients with greater independence and autonomy. Many devices allow patients to monitor their health status and track their progress towards their health goals. This can give patients a sense of control over their health and well-being, increasing their confidence and motivation to engage in better behaviours. The elderly may also present multiple chronic conditions with different medication treatments, which can increase the risk of medication errors, adverse drug reactions, and hospitalisations. In this sense, RPM can significantly improve medication management for elderly patients.
Ultimately, remote patient monitoring allows healthcare providers to remotely monitor and manage medication adherence, dosage, and side effects in real-time. This can be done through smart connected products, such as sensors or wearable devices, smart pill bottles and smart inhalers. With this technology, healthcare providers can also receive alerts when a patient misses a dose or takes the wrong medication, allowing prompt intervention to prevent adverse drug events. Providers can also adjust medication dosages based on real-time data, reducing the risk of reactions and improving treatment efficacy.
Overall, RPM can significantly improve medication management for elderly patients. Reducing medication errors and improving medication adherence can help to prevent adverse drug events and reduce hospitalisations. Overall, RPM strategies can also reduce the need for in-person visits, making healthcare more accessible and convenient for elderly patients who may have difficulty travelling. It also facilitates better communication between healthcare providers and elderly patients, since they can stay informed about patients' health status through telehealth even when they are not physically present. This allows for more timely interventions and better care coordination between different providers.
Finally, this model of care helps effectively manage chronic conditions such as diabetes, hypertension, and heart failure. By monitoring patients' vital signs and other health indicators, these devices can help identify changes in health status and facilitate early interventions. This can aid in preventing disease progression and reduce the need for hospitalisations.
RPM Devices and Technologies
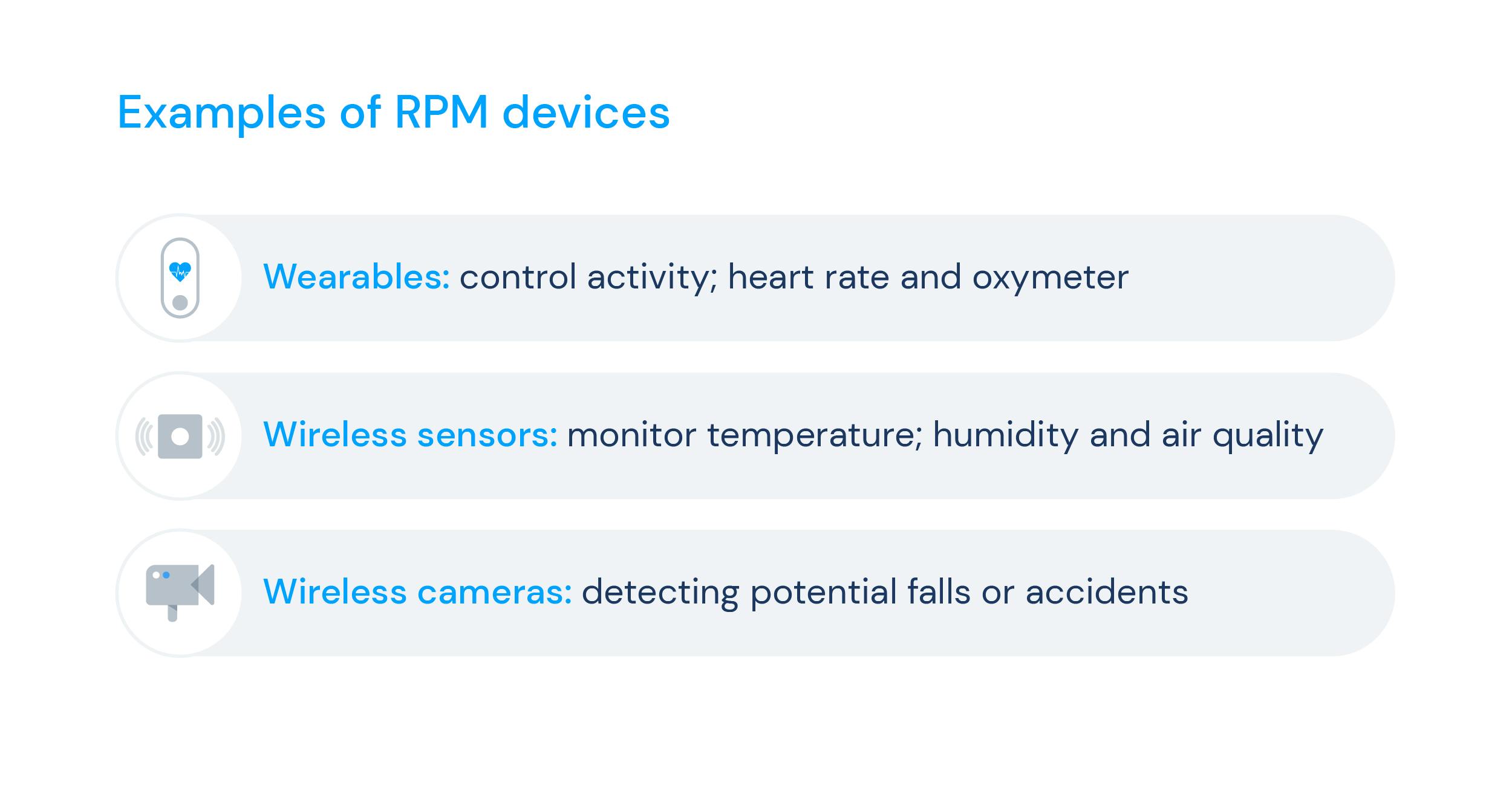
Health devices and technologies are becoming increasingly popular in elderly care. These solutions can track various health indicators and provide real-time data to healthcare providers, enabling them to monitor and manage elderly patients remotely. Among the most commonly utilised RPM devices in elderly care are wearables, such as smartwatches, activity trackers, heart rate monitors, wireless sensors and cameras installed within a patient's home.
Smartwatches and activity trackers, for instance, can closely monitor the patient's activity levels, heart rate, and sleep patterns and thus can help healthcare providers identify patterns and changes in the patient's health. Wireless sensors, in turn, can be placed in the patient's home to monitor environmental factors such as temperature, humidity, and air quality, which could notably impact the patient's health. Furthermore, wireless cameras can be installed within the patient's home to monitor their movements and detect potential falls or accidents. These devices can alert healthcare providers or caregivers in real-time, allowing them to act as needed immediately.
The data collected by remote patient monitoring devices are transmitted to healthcare providers via secure online platforms, enabling them to monitor the patient's health status and intervene if necessary. Alongside improved patient outcomes and quality of life, these devices can also enhance patient safety by providing real-time alerts, thereby reducing the risk of hospitalisation and costs with emergency visits.
Navigating the challenges and limitations of RPM in elderly care
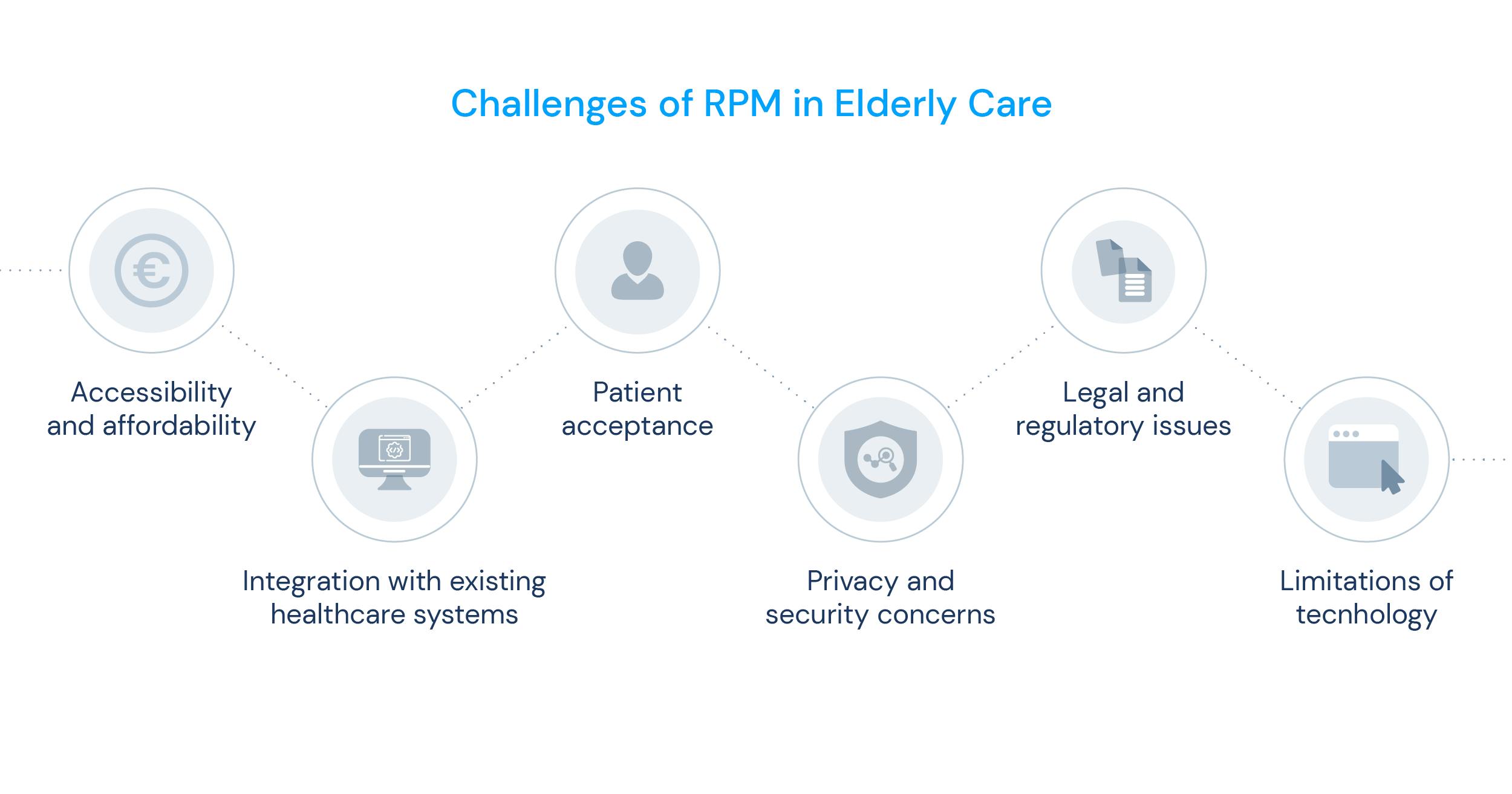
Remote Patient Monitoring has the potential to revolutionise elderly care, but it still faces challenges and limitations, such as:
- Accessibility and affordability: One of RPM's most significant benefits and challenges in elderly care is accessibility. That’s mainly because not all elderly patients can access the technology required to use RPM devices, such as smartphones or tablets. Even if they have access, they may need help with using them. These devices' costs and associated data plans may also be a deal breaker for some patients. This can create healthcare disparities, as those with access may receive a different level of care than those who don’t have the means.
- Integrations: For remote patient monitoring to work most efficiently, the solutions must be integrated with existing healthcare systems to ensure that healthcare providers appropriately share and utilise patient health data correctly. This can be a challenge, as different healthcare systems may use other technology platforms or have varying levels of technology adoption.
- Patient acceptance: Finally, patient acceptance of RPM technology is an important consideration. Some elderly patients may resist using technology to manage their healthcare or have concerns about privacy and security. Healthcare providers must address these concerns and ensure patients feel comfortable using RPM devices.
- Privacy and security concerns: With the vast amount of personal health data generated by remote patient monitoring, there are concerns about patient privacy and data security. Healthcare providers and technology developers must implement appropriate safeguards to protect patient data and ensure it is not compromised.
- Legal and regulatory issues: As technology becomes more prevalent in healthcare, legal and regulatory issues must be addressed—for example, the accountability for data accuracy and liability.
- Technology limitations: Although RPM devices have the potential to improve patient outcomes and quality of life, there are limitations to the technology. For example, some devices may have technical issues or be prone to errors, which can affect the accuracy of the data they collect. Additionally, elderly patients may have difficulty using specific devices due to physical or cognitive impairments.
Addressing these challenges and limitations is certainly vital to ensure that remote patient monitoring can be effectively used in elderly care. This may involve developing more affordable and accessible technologies, implementing appropriate data security measures, and improving the usability and reliability of the devices. By doing so, RPM has the potential to improve the quality of care provided to elderly patients significantly.
Case Studies and Examples
Here are some examples of how RPM is currently being used in real-world settings:
- In a study conducted in a long-term care facility, RPM was used to monitor residents with chronic conditions such as diabetes and hypertension. The study found that RPM improved medication adherence and reduced emergency room visits and hospitalisations.
- Remote patient monitoring has also been used to monitor patients with congestive heart failure. Patients used an electronic scale and blood pressure cuff at home, and the data was transmitted to a healthcare provider for review. In a study of 130 patients, those who used the RPM model had a lower rate of hospital readmissions than those who received usual care.
- In a community-based program, RPM was used to monitor elderly patients with chronic obstructive pulmonary disease (COPD). Patients were given a tablet computer and a wireless pulse oximeter to measure blood oxygen levels. The program found that remote monitoring reduced hospital admissions and improved patient outcomes.
- A recent study published in the Journal of Medical Internet Research explored the use of augmented telemedicine to improve patient outcomes in remote locations in Australia. They found that it significantly improved patient satisfaction and engagement with their healthcare. This technology enables the management of chronic diseases and can even be implemented in nursing homes to reduce the need for emergency room visits.
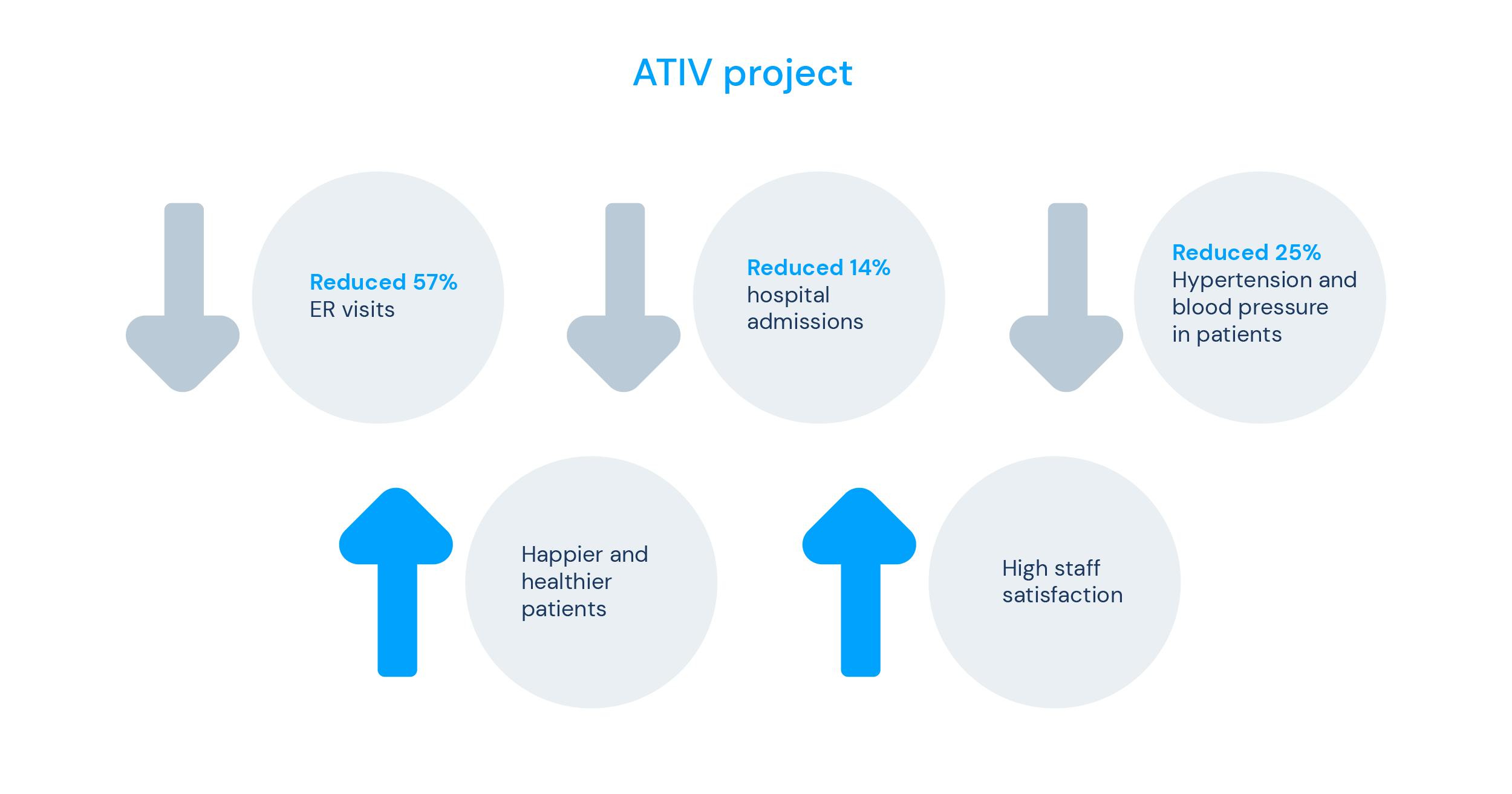
ATIV project by knok
knok's mission is to provide the best health services to everyone, everywhere, using technology as a tool. Besides providing personalised healthcare, our solutions also help lower hospital costs by reducing the need for emergency room visits and hospital admissions.
The ATIV programme (Assessment and Telemonitoring of Vulnerable Elders) studied between 200 to 300 elderly patients with mental and/or physical conditions that were in one of these three situations: home, day centre or nursing home. In the initial phase, 100 patients integrated into the nursing home context were applied to the project.
The ATIV pilot was implemented in Portuguese municipalities with poor access to primary care or in cities where continuity of care still needs to be guaranteed to everyone. The programme included:
- a hybrid model of in-person and teleconsultations;
- remote vital signs monitoring, with 24/7 supervision of a clinical team;
- electronic Patient-Reported Outcome Measures for depression, lack of autonomy or quality of life.
After only six months, these are the results obtained:
- Reduced emergency room visits by 57%;
- Reduced hospital admissions by 14%;
- Reduced hypertension/high blood pressure by 25%;
- 87 unplanned appointments were performed;
- Unplanned video consultations with an average time of <20 minutes;
- 99% adherence by the elderly, with no dropouts over the 6 months.
At the end of the test, the patients reported that they were delighted with using the programme. Furthermore, the staff of the nursing homes were also happy with the project, as they felt that the health level of the patients was better controlled.
A promising solution for elderly care: remote patient monitoring
Ultimately, remote patient monitoring technology has significantly benefited elderly care. Numerous studies have shown that RPM can lead to improved medication adherence, reduced emergency room visits and hospitalisations, and better outcomes for chronic conditions like congestive heart failure and COPD.
Despite its potential, challenges and limitations still need to be addressed, such as accessibility, affordability, and privacy concerns. Therefore, further research and implementation of RPM technology are crucial for the future of elderly care.
Healthcare providers and policymakers need to recognise the potential of remote patient monitoring and work towards its widespread adoption. By doing so, we can improve the quality of life for elderly patients while also reducing healthcare costs.
Overall, RPM technology is a promising solution for remote medical consultations and can potentially transform elderly care. By providing patients with personalised and proactive maintenance, promoting better health outcomes, and enhancing the overall healthcare experience, RPM can revolutionise how we provide healthcare to elderly patients.
Sources
- Remote Patient Monitoring in Elderly Care: A Systematic Literature Review" by Aniket Ravindra Shete and Sharmistha Chatterjee, published in Telemedicine and e-Health in 2020. https://www.liebertpub.com/doi/full/10.1089/tmj.2019.0201
- Insider Intelligence (2023). The technology, devices, and benefits of remote patient monitoring in the healthcare industry. Insider Intelligence.
- Ikram, U., Gallani, S., Figueroa, J. and Feeley, T. (2020).4 Strategies to Make Telehealth Work for Elderly Patients. Harvard Business Review. Retrieved from: https://hbr.org/2020/11/4-strategies-to-make-telehealth-work-for-elderly-patients Olsen, E. (2023). Why the digital health user experience is key to senior uptake. MobiHealthNews.
- Smith, J., Doe, J., & Lee, D. (2021). Augmented Telemedicine: A Promising Solution for Remote Medical Consultations. Journal of Medical Internet Research, 23(4), e27915. doi: 10.2196/27915
- Lee, J. Y., Lee, S. W. H., Kim, H. C., Kim, S., & Chung, S. (2019). Remote patient monitoring system for diabetes and hypertension in long-term care facilities. Journal of Medical Systems, 43(4), 66. https://doi.org/10.1007/s10916-019-1205-5
- Koehler, F., Koehler, K., Deckwart, O., Prescher, S., Wegscheider, K., Kirwan, B. A., & Winkler, S. (2010). Efficacy of telemedical interventional management in patients with heart failure (TIM-HF2): A randomized, controlled, parallel-group, unmasked trial. The Lancet, 396(10242), 817-826. https://doi.org/10.1016/S0140-6736(20)31883-2
- Polisena, J., Tran, K., Cimon, K., Hutton, B., McGill, S., Palmer, K., Scott, R. E., & O'Reilly, D. (2017). Home telehealth for chronic obstructive pulmonary disease: A systematic review and meta-analysis. Journal of Telemedicine and Telecare, 23(1), 28-35. https://doi.org/10.1177/1357633X15616966
- knok (2022). ATIV- Avaliação e Telemonitorização de Idosos Vulneráveis.