
Improving primary care through the digital lens
Read more about the importance of digital primary care for a more accessible healthcare system.
The foundation of any healthcare system is its frontline troops: primary care forces. Even in a digital-powered society with such advanced technology and new procedures, primary care is still crucial since it’s the first point of contact with the patient.
In primary care, digital technologies have been and continue to be widely adopted and scaled, especially in the last two decades. This department is vital to delivering quality healthcare, improving patient health and well-being, and efficiently functioning a health system under constant and increasing pressure. However, such rapid digitisation, multisystem connectivity, and the growing collection of sensitive digital data also emphasise the increasing importance of a virtual healthcare environment. According to the World Health Organisation (WHO), primary care is based on five core functions:
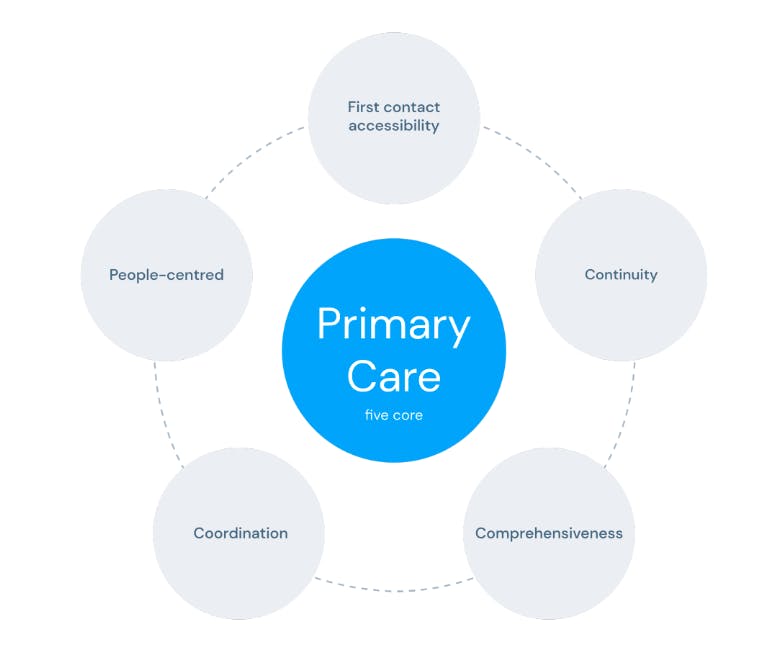
It aims to improve the population’s overall well-being while reducing disparities in access to health services or healthcare needs. These core functions in primary care work are:
- Establishing a first point of contact enhances access to health services;
- Fostering the growth of long-standing personal connections between patients and healthcare providers or primary care physicians;
- Providing extensive services, including preventive, promotive, curative, palliative, and rehabilitative care, is vital to comprehensiveness;
- Coordinating streamlined services and care delivery across various levels of the healthcare system over time;
- Emphasising patient-centred care that involves educating and supporting individuals in making informed decisions and actively participating in their care.
Healthcare for everyone, everywhere
There’s no denying that digital health came to stay. It has become an essential part of the healthcare industry. Improving and automating processes are just some of the benefits of digital health, and they can be highly beneficial to primary care physicians. Augmented telemedicine, for example, can also be a valuable resource for digitising primary care.
Primary care isn’t just the first point of contact with patients. It also englobes the mission to optimise health processes and provide equal healthcare access to reduce health disparities by ensuring everyone receives the best care possible everywhere. While this is a conceptual definition of a perfect world, accessibility to healthcare presents different scenarios in each country. This mission is even more pertinent in today’s society of disparities. Digital health solutions make it possible to deliver optimal primary care everywhere. The US National Academies of Sciences, Engineering, and Medicine (NASEM) has developed an approach of suggestions for implementing high-quality primary care. The committee defined it as “the provision of the whole person, integrated, accessible, and equitable healthcare by interprofessional teams accountable for addressing most of an individual’s health”. It recommended two main groups of actions:
- projects with a patient-centred care focus;
- the adoption of “a comprehensive aggregate patient data system”.
The first aims to humanise healthcare to defocus from “disease care” and take the term ‘healthcare’ literally – meaning making sure that patients are monitored and have regular health check-ups rather than just treating them when there’s a condition already in place. While the second one encourages the creation of a system that allows doctors and patients to view personal health records easily, an optimising time during consultations and treatments.
Telemedicine is a digital health solution that can provide easy medical monitoring and healthcare access to those who cannot afford it due to geographical or social-economic reasons. With Augmented Telemedicine, the patient journey is entirely digital: from a first contact triage process to an AI symptom checker and vital signs reader to a final online consultation with a doctor. All data collected is saved as health insights.
The second point mentioned by the NASEM brings up an honest discussion about one of the significant concerns related to digital health: cybersecurity and data privacy. Although it’s something relatively new, the usage of big data in the healthcare industry has already proven that it can benefit the sector's technological advancements. With AI, computer and machine learning, and advanced health data analytics, it’s possible to collect data and create value for healthcare providers, thus improving overall patient care. As this is a more sensitive topic due to the compliance and legal aspects in place, it’s necessary to work towards a model that certifies and secures all personal data.
Protecting Data in a Digital Health Environment
Data has become a big piece of the puzzle of digital healthcare in the same way it has revolutionised other industries. Data is everywhere and anywhere right now, but the usage and application of big data has explicitly played a significant role in the healthcare sector, opening up a whole new world of possibilities to explore.
As healthcare is turning more digital by the hour, the use of data in a medical setting has enormous potential for all providers. One of the significant challenges when managing big data in healthcare is combining all different data sources in an easy, comprehensible way. However, it’s essential to be aware of data protection, privacy, and safety.
Cybersecurity is Sine Qua Non
The unprecedented demand for primary care services driven by the COVID-19 pandemic and an ageing population made digital health solutions expand to Electronic Health Records (EHRs), allowing practitioners to share data and enhance care delivery.
However, this exponential cause-effect growth of digital health and access to patient information has created a much greater risk for data breaches and cyberattacks. Due to the sensitive nature of clinical and patient data, healthcare providers, health insurers, and physicians must be cautious and knowledgeable about the risk of all cybersecurity and data privacy threats.
The ENISA 2020 Data Breach Threat Landscape report states that the number of cyber breaches has increased by 54% by mid-2019 compared to 2018. The report further states that:
- 71% of the data breaches were financially motivated;
- 52% of data breaches involved hacking;
- 70% of breaches exposed personal details from emails, such as date of birth.
Also, apart from data breaches, phishing attacks that deliver malware to applications or systems are another way attackers download data. As more than half of European citizens are concerned about their data security, access and sharing, these numbers are also alarming to healthcare.
How to secure Digital Health Data
Healthcare providers and solution developers should take this concern as a motivation to create systems that offer data protection and security while enabling the same data to be shared and providing insights for healthcare organisations. As soon as providers can incorporate all patient-related data, physician’s observations, health records, diagnostic exams, and real-time data in one secure place, insights will be more effective in helping deliver value in healthcare. To build such solutions, it’s essential to keep in mind the following topics:
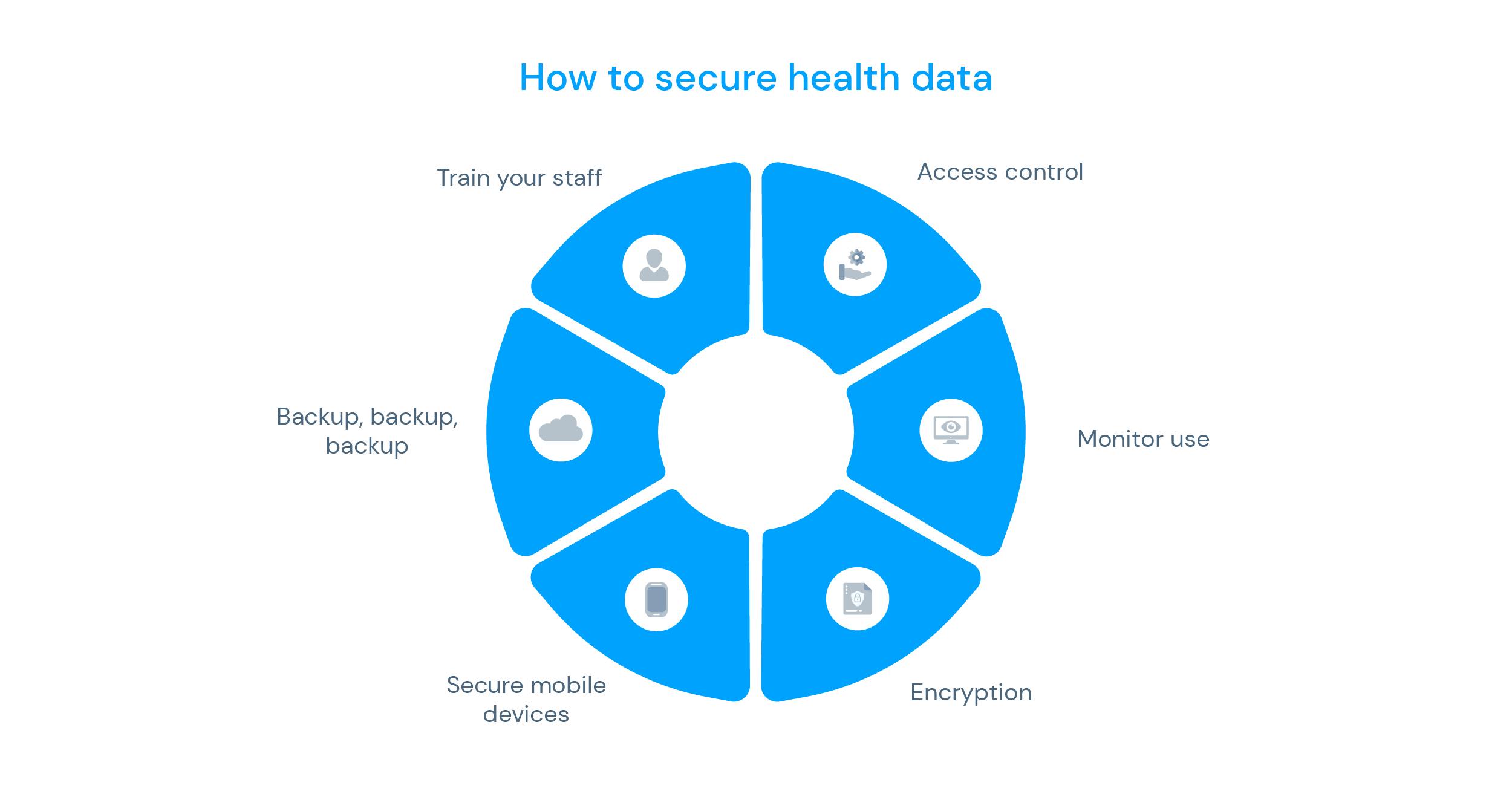
1. Access Control
It might seem obvious, but it’s essential to determine and control who has access to digital health data. This can be done by creating role-based permissions that give healthcare organisations control over who can access data. Only those who work with specific data types should be able to see and/or use them to prevent data breaches.
2. Monitor Use
Providers should have a system that allows them to monitor activity within their systems; for example, tracking logs in, frequency of logins, and using data and applications. This control is vital for auditing, inspections and monitoring of unusual activities.
3. Encryption
Encrypted data is a no-brainer when discussing cybersecurity since information becomes useless in a cyber attack unless they have a decryption key to make it readable. Ensuring health providers are encrypted is the best way to protect patients’ health data.
4. Secure Mobile Devices
Another strategy for a secure digital health environment is corporate-owned devices instead of a bring-your-own-device environment. With this protocol, it’s possible to standardise and manage solutions centrally, allowing providers to choose devices that enable biometric user authentication, making them inherently more secure.
5. Backup, backup, backup!
Don’t overlook the importance of building a comprehensive backup and data recovery strategy. Healthcare organisations must create and store recoverable backups on different media types and locations, with at least one air locked or offline, so that data is always accessible.
6. Train your staff
Similar to simulating fire situations, it is essential to have a well-trained staff that understands the security regulations and processes to protect the data and its users. More than just having a team exclusively dedicated to it, training employees on digital health data protection is a golden rule.
Interoperability is a must-have
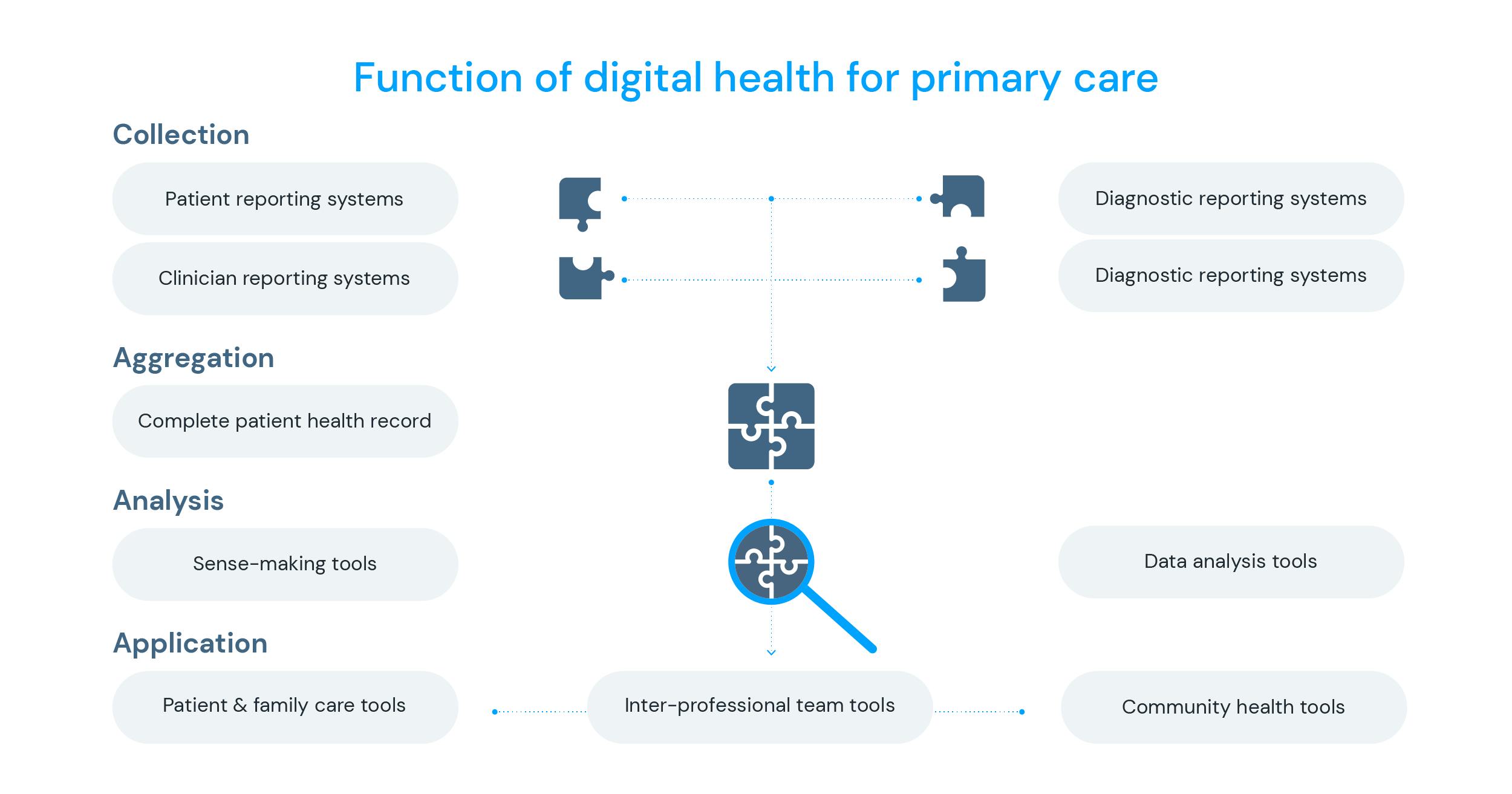
In primary care, digital health can present itself in many tools such as EHRs, patient portals, mobile applications, telemedicine platforms, electronic registries, analytic systems, remote monitoring, wearable technology and devices, care team communication support, and geographical or population health displays. These must follow certain design principles for digital health systems and implementation strategies to ensure they support high-quality primary care.
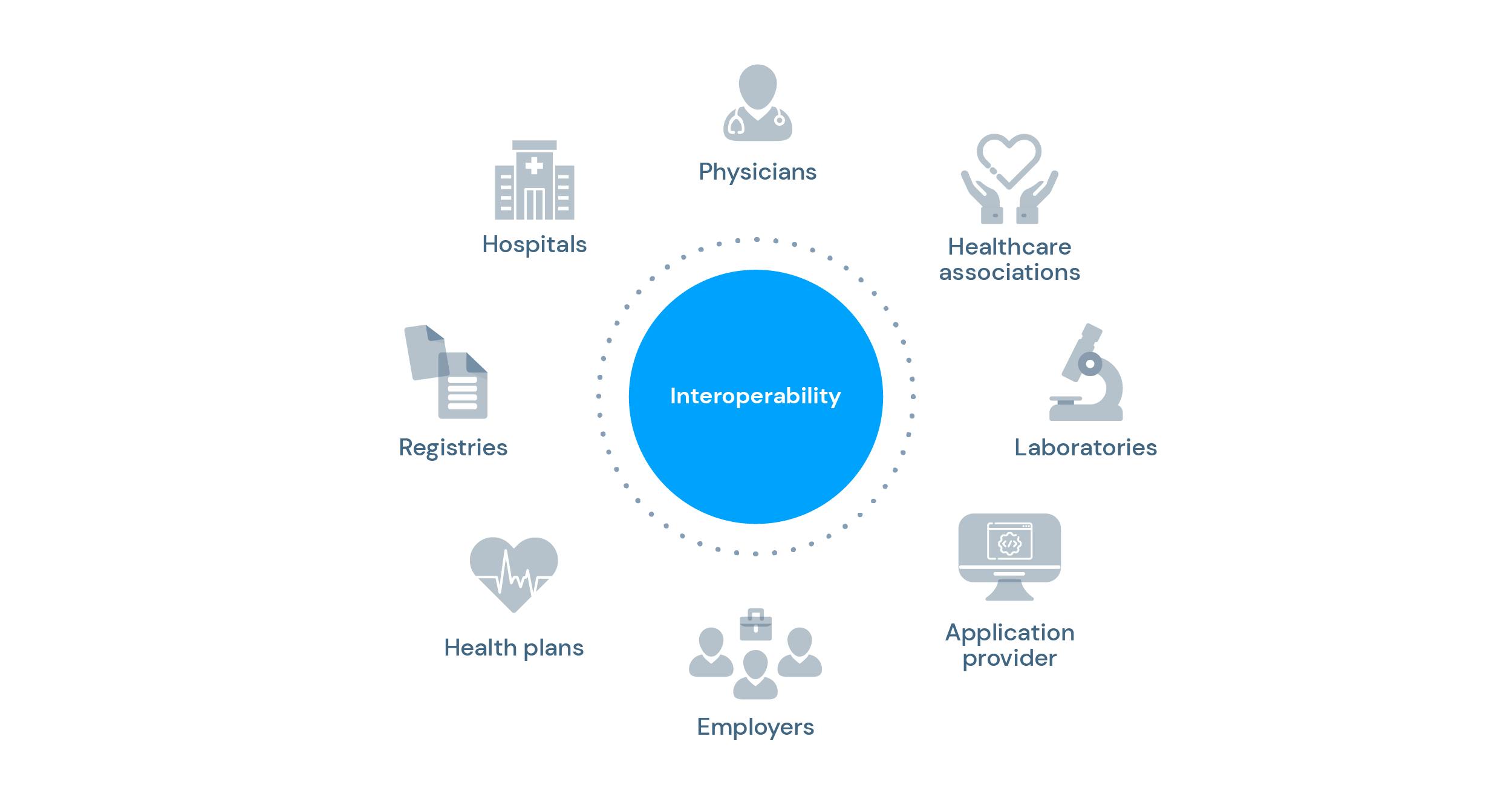
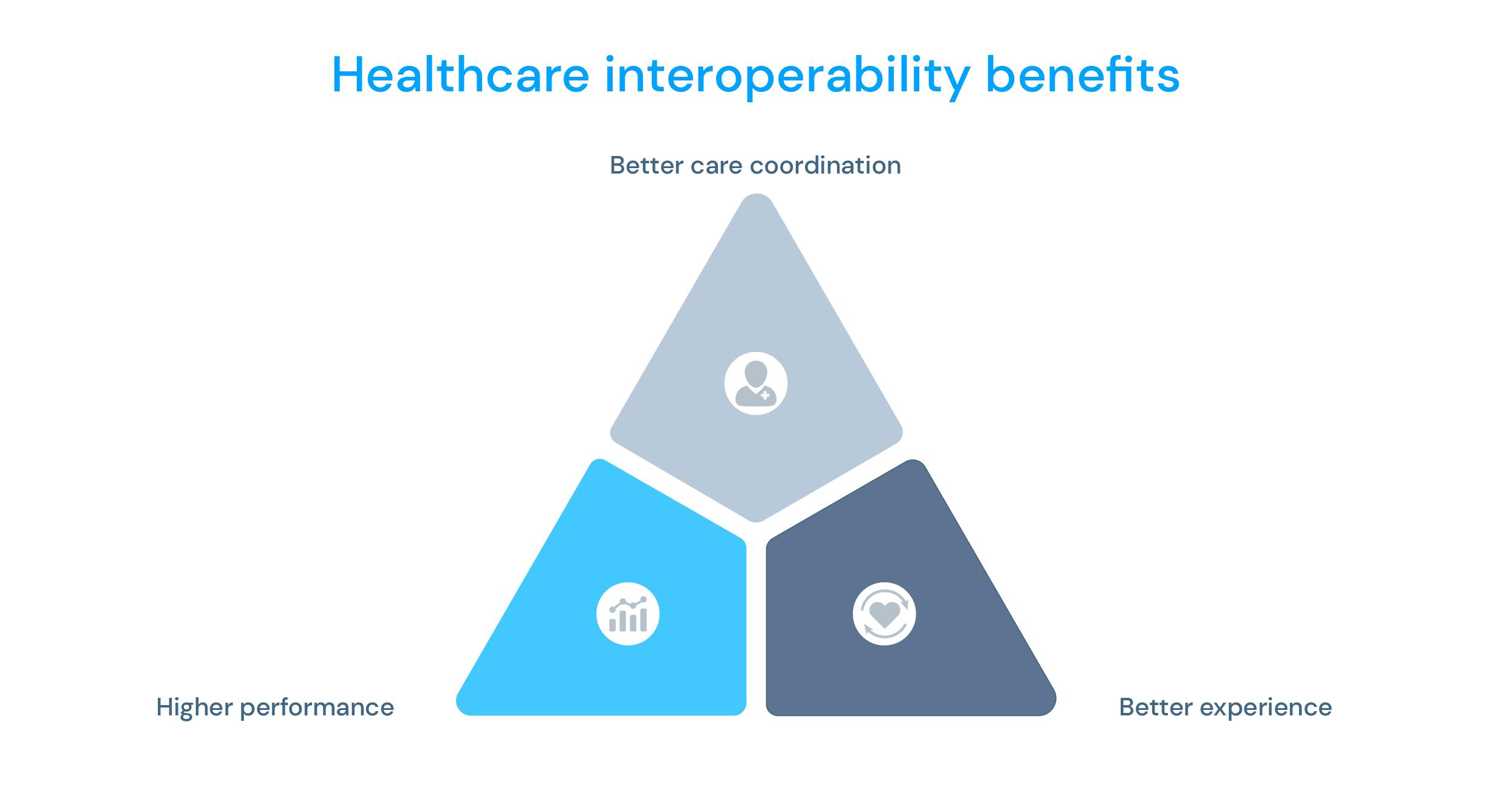
As populations grow older and people live longer, interoperability and data sharing are critical for efficient healthcare delivery. With many providers having a digital information system, it’s imperative to have a net with all patient-related data integrated with hospitals, clinics, and medical centres.
Improved interoperability would allow organisations to break free from viewing individuals as occasional patients' health plan members or customers. This shift would enable industry decision-makers to concentrate on analysing people's access and utilisation of health information, regardless of its origin, to enhance care delivery models, promote patient safety, and enrich the experiences of those they serve. To ensure interoperability is an existing practice, some standards are frameworks already being developed and optimised, such as HL7 and FHIR, presented below.
- HL7 Medical Standard
Widely used in medical-information communication, Health Level Seven (HL7®) is a standard guideline that facilitates the exchange of information between medical information systems. Encompassing various functional domains, it plays a vital role in attaining interoperability in healthcare. This standard is at the intersection of healthcare, engineering, and Information Technology (IT). It covers almost all functional domains encountered in healthcare related to patient management and administration, order management, and observation reporting.
Professionals involved with information technology in the healthcare sector are required to possess a thorough understanding of HL7. Providing APIs that support interoperability and with features like EHR systems in an Augmented Telemedicine setting, knok is an HL7 affiliate and showcases a fully integrated patient experience.
- FHIR
Acronym for Fast Healthcare Interoperability Resources, FHIR is an open-source healthcare data framework developed and nurtured by HL7 standards. FHIR was created to make it easier for healthcare data to move from one system to another – allowing interoperability. It organises data into resources and creates a standardised structure for collecting, using, and storing data. FHIR can also operate financial and workflow data, such as claims information, appointments, etc.
All hands-on cybersecurity
Digital healthcare applications have shown their potential to reduce inefficiencies in delivery, access, and costs while improving quality and growing the concept of medicine to a more tailored and precise service. Prevention continues to be a key approach and ally to digital health, which has also proven cost-effective in the long term. More vulnerable populations can transform their quality of life by improving access to health and care, creating a more equal and healthy society overall.
At knok, we developed the concept of Augmented Telemedicine as an enabler to support continuity of care, which serves as a base for our work frame. This concept is carried throughout our white-label telemedicine platform – Panacea. Panacea’s data functionalities can change how healthcare providers generate new and secure solutions while improving their patients’ health.
Fully GDPR-compliant and anonymous unique data collection allows the creation of clusters based on more than 150 data points to identify risks and behavioural patients patterns. knok will also soon provide an ISO 27001 certification, a significant achievement for information security management. All in all, knok offers a fully integrated and secure telemedicine solution that delivers preventive and continuous care to everyone, everywhere.